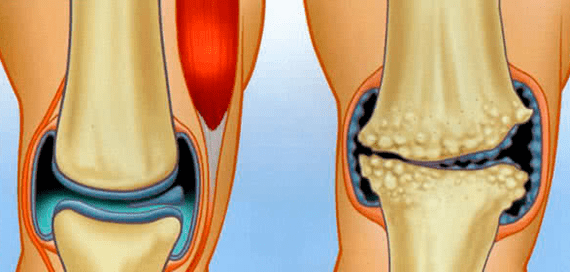
The surfaces of the bones which form the joint are covered with a special hyalin cartilage - smooth, offering the lowest friction force during the motor skills of the surfaces appearing.If osteoarthritis is diagnosed, this means that cartilage is destroyed.
By progressing, the destructive process applies to bones, then to the joint capsule.The disease has a universal code according to the CIM 10-M15-M19, by counting it in the class of pathologies of muscle tissue and bone connected.
According to medical statistics, 12% of the world's population suffers from osteoarthritis, most of which are 65 years old.However, each year, there is an alarming trend to increase the number of young people.The diagnosis is not deadly, but osteoarthritis is insidious with its relapses and the threat of total handicap.
The occurrence mechanism
The disease is developing gradually, four stages can be distinguished conditionally:
- Initially, an ill -supplied area with blood or damaged appears on the cartilage area.Little by little, in the presence of traumatic factors, the region is not restored, but, on the contrary, develops.
- The body, trying to restore destructive cartilage, replaces damaged areas with a mineralized tissue that has no clear structure.Such a fabric is, in general, with a lower replacement for smooth, slippery and elastic hyalin cartilage.
- Gradually, the surface of the cartilage becomes in scars and bone growth - osteophytes.
- The healthy areas of the load have increased several times, wear very quickly and, therefore, the entire cartilage turns into a large scar.
If the pathological process is not stopped, the joint will undergo the following unfavorable changes:
- The bones are involved in the destruction process;
- The synovial shell is ignited;
- The joint capsule becomes denser, losing its elasticity;
- The light of the joint difference decreases rapidly;
- The bones, without friction resists, are distorted, as the joint as a whole;
- The tissues of the articulation are reborn, there is therefore a complete loss of the possibility of movement.
Types of osteoarthritis
This disease absolutely affects all joint surfaces!At the same time, despite the same pathology mechanism, it is classified into several types.
Thus, according to the sick joints, they distinguish:
- osteoarthritis of the knee joint or the Patellofmoral osteoarthritis (abridged gonartrose);
- osteoarthritis of the hip joint (abridged coxarthrosis);
- osteoarthritis of the shoulder joint;
- interfanating arthritis;
- osteoarthritis of the ankle joint;
- Hand osteoarthritis;
- cervical osteoarthritis;
- arthritis of the jaw;
- osteoarthritis of the plusnephalanx joint;
- iliac arthritis;
- Keywriter-secondary arthritis;
- temporal osteoarthritis;
- heel osteoarthritis;
- arched osteoarthritis which affects arc processes of the vertebrae (abridged spondylarosis);
- osteoarthritis of the articulation of the facets of the joints of the spine;
- Non -Kovevertural osteoarthritis;
- osteoarthritis of the preliminary coasts;
- Taran-plastic osteoarthritis.
Depending on the specifics of the pathological process in the cartilaginous tissue, they distinguish:
- Distorting osteoarthritis is the name of the disease that has gone to the terminal stage (final);
- Arthrosoarthritis - The presence of the classic inflammatory process is characteristic;
- chronic;
- Acute osteoarthritis.
For the reasons for the occurrence of pathology, they distinguish:
- Dystrophic arthritis of the joints associated with a critical metabolic disorder;
- Fracture osteoarthritis is caused by appropriate injuries;
- Post-traumatic arthritis.
There is another classification - by the question of whether the disease is independent or caused by provocative factors:
- The primary, - occurs on a completely healthy cartilage, another name - idiopathic osteoarthritis, or appears with senile changes linked to age;
- Secondary, caused by many reasons.
Osteoarthritis
There are signs of osteoarthritis rather typical of all the locations which, according to the degree of development of the pathology, differ in their gravity:
- Evils, pain, intensification with high humidity and hypothermia;
- decrease in joint mobility;
- Crisp, creaky and crossed sounds in the movements of joint surfaces;
- external changes in the contour of the joint;
- swelling and swelling;
- redness of the skin.
Pain
The very initial signs of violations are felt by small or moderate and short -term pain, which almost never occurs at night, but generally appears only with a load on the articular surface.
When the inflammatory processes moved to his last step, the patient begins to feel unbearable, the pain "gnawing" due to the stagnation of the blood and the increase in pressure in the joint bag.The pain is characterized by a long time, at any time of the day, and that the affected area is in the rest or in motion.
Joint sowarity
This symptom is characteristic of a fairly neglected disease.At the same time, in the first stages, the patient always feels in the morning, after waking up, discomfort when he moved in the form of a feeling of constraint.
With the progression of destructive reactions, the patient remarks:
- Restriction of the amplitude of usual movements;
- The inability to change the position of the members at rest, even making attempts to manually sef the joint;
- Strong fixation (contracture) in a certain position of the articulation, which for a long time was in a state of lack of motor activity.
In the end, in the fourth stage of pathology, an anchilosis is formed in the form of replacement of the articular tissues in scars, with a complete loss of functionality.
Sounds in the joint
A crunch can be accompanied by any dysfunction of bones and cartilage, not only caused by osteoarthritis.
However, this disease is characteristic that sounds:
- only occurs in the articulation that hurts;
- accompanied by movement difficulty;
- He has the ability to intensify with the progression of pathology and comes across the formation of an anchilosis.
Change the appearance of the joint
Notable changes appear in the subsequent stages.Thus, the axis of the affected limb is curved, and the joint region itself is disfigured - it grows in size, the shape is ugly modified.
All this indicates an irreversible destruction of the joint, inside which a new fabric has not been formed, not having a certain structure.
If such a pathogenic process has appeared in the knee, this means that the charging and the more noplange joints will increase the load on the ankle joints, which will also damage them over time.
The causes of osteoarthritis
Pathology can occur both in a single articulation and distributed with several.This disease is the least likely to occur at a young age - vitality is still sufficient for self -scoring of the body.
However, for all age groups, the causes of influence in their direction are: there is:
- Internal - certain diseases, bad habits, unbalanced nutrition, etc.;
- External, - injuries, professional factor.
Internal causes cause a negative change in joint factors in the form of joint inflammation.Distinguish between inflammations of various origin:
- infectious (intestinal wand and koch wand, viruses, chlamydia, staphylococci, pale thirtema, etc.);
- rheumatism;
- purulent arthritis;
- autoimmune nature;
- drop;
- psoriasis.
In addition, the causes of internal exposure include congenital or acquired violations of the structure of the cartilage and malnutrition fabric, which can be associated with:
- Genetic dysfunctions and mutations;
- Intrauterine development anomalies, including perinatal injuries;
- old age;
- osteoporosis, that is to say the "leachate" of the bone tissue of the components of the elements;
- Hormonal disorders and overload, including menopause;
- violations of normal metabolism;
- disadvantage in the nutrition of vitamins and trace elements;
- Diseases that attract muscle weakness;
- Prolonged internal poisoning.
The worsening of many diseases of the musculoskeletal musculoskeletal also involves degeneration of cartilage.
The external causes of the development of the disease are factors that damage the joint such as:
- frequent hypothermia;
- dislocations;
- Strong blows;
- fractures;
- Meniscus injections;
- strong physical activity (weight lifting, for example);
- Professional sports;
- Joint surgical intervention.
Degree of osteoarthritis
According to clinical manifestations and the process of progression of the disease, four stages of osteoarthritis are distinguished:
- Osteoarthritis of the 1st degree, this is the initial stage of osteoarthritis, which is characterized by symptoms hidden in the form of negative changes in the composition of the synovial fluid and the weakening of muscle fibers, if it appears, then only with physical effort;
- 2nd degree osteoarthritis - it is already a feeling of pain due to the destructive bone joint and the formation of osteophytes, reflex neurotrophic regulation is disturbed and an audible crunch appears;
- 3rd degree osteoarthritis is characterized by significant degenerative changes in the joint, its visible deformation with the curvature of the limb axis, the ligament is shortened and the joint becomes pathologically mobile;
- 4th degree osteoarthritis is complete ankylosis, complete contracture and severe pain even at rest.
The four stages take place unevenly: during the pathological period, net exacerbations and moments of remission are possible.
Osteoarthritis
It is clinically proven that treatment and prevention in the form of elimination of provocative factors for damage to hyalins, although they do not eliminate the disease at the initial stage, but stop its development and restore the functionality of the joint.
Basically, the disease of small and moderate severity is treated with conservative methods.In the case of a serious destruction of the cartilage, which involved the destruction of the bones, the surgical endoprothetics is indicated.
In addition, the basic principle of treatment is:
- A complete approach involving the use of several therapeutic methods;
- Determination, that is to say the concentration of efforts on the elimination of the disease, causing the disease and the consequences.
Treatment with folk remedies
It is treated in depth, but at home, you can also use healing recipes for healers who offer effective treatment for health problems through herbs and beekeeping products.
Of the use of plants:
- Bay Leaf in the form of decoctions, dyes on vodka and specially prepared oil used outside, directly in the inflammation area;
- The treatment of osteoarthritis with honey has been established as a reliable local potion, in the form of rubber inflammation and nourishing the skin, muscles and cartilage;
- Cabbage leaf - Better than white cabbage - it is a little sick, and they wrap it with a painful stain, isolated with a wool fabric on top, and hold over the night;
- aloe juice in the form of compresses and friction in the skin;
Also helps the burdens of osteoarthritis of the knee articulation: the sheet is bandaged at the painful point, which is isolated throughout the night.
Preparation of osteoarthritis
The drug treatment linked to the classic method of therapy is divided, according to the dose form used, in drugs:
- External use, in the form of an ointment for osteoarthritis, friction, lotions;
- injections;
- osteoarthritis pills;
- Capsules.
Wave
The pharmacological industry produces medical ointments based on natural and very active components:
- Vishnevsky ointment;
- Heparin ointment.
The Vestaren tool containing 1% of Diclofenac helps well: the Voltaren in the form of a frost is applied to the skin.
Injections
The injections not only intravenously and intramuscularly, but also directly in the damage area, for example, the drugs of the non -steroid group, have proven itself in the treatment.
Thus, intra-articular injections are introduced into damaged joint tissues:
- The glucocorticoids that improve nutrition of the cartilage fabric that relieve inflammation and increase elasticity - Diprospan, Hydrocortisone, etc.
- Chondroprotectors and analogues of intra -articular liquid, - Singial, carbon;
- Hyaluronic acid as lubricant and analgesic.
Preparations in the form of tablets and capsules
SO chondroprotectors called for osteoarthritis containing structural elements of hyalin cartilage are in medicinal therapy and restore it in this way.
These drugs are produced in the form of tablets and capsules intended for oral administration through the gastrointestinal tract (orally).In addition, patients are prescribed by NSAIDs - anti -inflammatory drugs for osteoarthritis of the non -steroid group, stopping acute pain and the relief of exacerbations.
Anesthetic agents are also used in the form of a blockade of novocaine.
In addition, complex vitamins prescribed for osteoarthritis.
According to natural drugs from local action, medical bile is recommended, applied in the form of skin compresses.
Osteoarthritis exercises
Special exercises and therapeutic gymnastics (exercise therapy), whose complex gives physical activity on the unhealthy part of the body sparingly, proven itself.
Dr. Bubnovsky and Evdokimenko have developed their own therapeutic exercise complexes.
Massage with osteoarthritis
Very beneficial affects treatment and medical massage, which improves microcirculation and nutrition of deep tissues.
Diet with osteoarthritis
In this state, it is important to join an appropriate rational nutrition in order to slightly improve the patient's condition.Recommended abstinence of overeating, exclusion of animal fats and fried foods.
What a doctor first treats Arthrosv with pain complaints in the bone joints should go to the therapist.It is he who, having summarized the history of the patient and asking him in detail, will refer to the desired close specialist.
This can be, depending on the cause of the disease and its type, profile doctors such as:
- Orthopedist;
- traumatologist;
- surgeon;
- rheumatologist.























